The Future of Customizable Hearing Aids
Hearing aids have evolved from basic amplification devices to
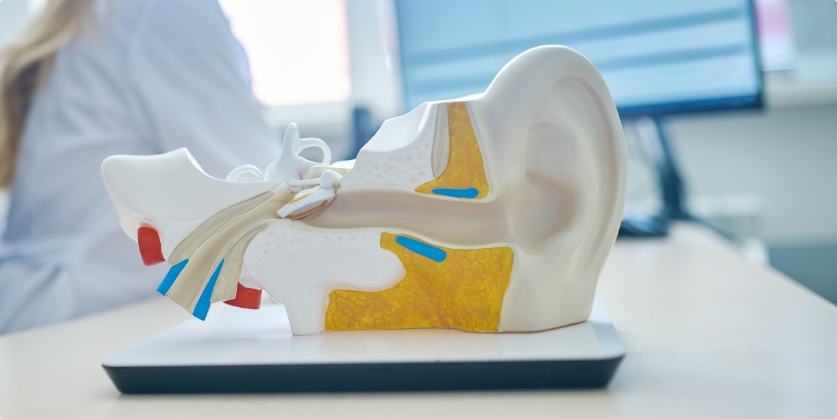

Hearing aids have evolved from basic amplification devices to
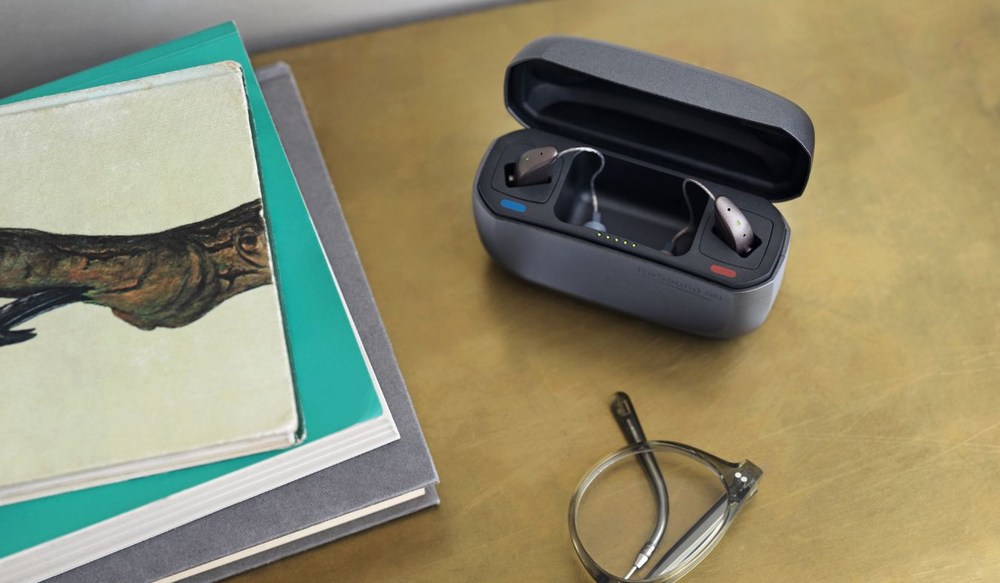
Your hearing aids can now work together with the same devices that count

Rob Hamilton and the team at Hearing Well Matters in Burlington have a